Corneal Infection
A wide variety of infectious agents can affect the cornea. The most common cause of corneal infection is a bacterial ulcer caused by poor contact lens hygiene. Sleeping in contact lenses, reusing cleaning solutions, and not using appropriate contact lens cleaning solution increases the risk of corneal infection 15x that of someone who cleans their contact lenses routinely and appropriately.
Signs of a corneal infection include:
- Pain
- Light sensitivity
- Decreased vision
- Tearing
- Discharge
If you experience these symptoms it is important to see your eye doctor immediately. We at VisionFirst Eye Center have extensive experience in successfully diagnosing and treating ocular infections.
Corneal Dystrophy
Corneal dystrophies refer to a group of bilateral, hereditary corneal disorders where substances deposit within the various layers of the cornea and accumulate over time. This often results in decreased vision and light sensitivity, but can also be painful depending on which layer of the cornea is affected.
Symptoms of a Corneal Dystrophy
Corneal dystrophies are generally diagnosed during a routine eye exam. Initially, you may not have symptoms, but the vision can gradually deteriorate with age.
There are over 20 different corneal dystrophies.
Though symptoms of each type will vary, all corneal dystrophies share these traits:
- They are hereditary, meaning it can be transmitted from parent to child
- They are not caused by factors such as injury or diet
- They usually progress slowly
- They affect both eyes
- Most can occur in otherwise healthy individuals
There are a variety of treatment options available for corneal dystrophies. Some dystrophies may be asymptomatic and can be observed. Others may require an in-office cornea procedure, laser vision correction, or corneal transplantation in order to restore vision.
Keratoconus
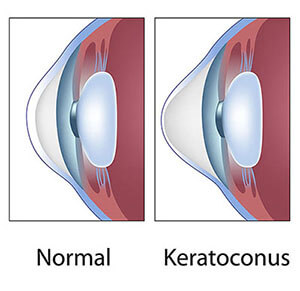 Keratoconus is a progressive disease that causes abnormal thinning and protrusion of the cornea. Keratoconus often causes decreased vision even with prescription glasses and rigid contact lenses may be necessary in order to obtain quality vision.
Keratoconus is a progressive disease that causes abnormal thinning and protrusion of the cornea. Keratoconus often causes decreased vision even with prescription glasses and rigid contact lenses may be necessary in order to obtain quality vision.
Keratoconus can often be diagnosed during a routine eye examination.
What are the treatments for keratoconus?
There are several treatment options depending on the severity of keratoconus. Specialty contact lenses may provide adequate treatment for stable disease, and corneal INTACS are a potential option for patients who are contact lens intolerant.
Corneal crosslinking has been FDA approved for the treatment of progressive keratoconus. During this procedure your doctor applies liquid Vitamin B2 (Riboflavin) drops to the cornea, followed by 30 minutes of UV light exposure. The combination of Riboflavin and UV light helps to strengthen the cornea and stop the progression of keratoconus.
When keratoconus is severe and visual quality is poor even with specialty contact lenses, the ophthalmologists at VisionFirst can perform corneal transplantation to restore your vision.
Corneal Scar
A scar on the surface on the cornea may result from trauma, infection, inflammation, rigid contact lens wear, and many other etiologies.
There are a variety of treatments depending on the location and depth of corneal scarring, as well as its impact on your quality of vision. At VisionFirst, we will assess the corneal scar and can recommend different treatment modalities including specialty contact lenses, laser vision correction, or corneal transplantation.
Pterygium
 A pterygium (ter-idge-ee-um) is a non-cancerous, triangular-shaped growth that begins on the white surface of the eye (conjunctiva) and spreads onto the cornea. UV sunlight exposure is the primary risk factor for pterygium formation and progression. A pterygium can cause foreign body sensation, irritation, tearing, and redness. These symptoms can be treated by eye drops or ointment prescribed by your doctor at VisionFirst.
A pterygium (ter-idge-ee-um) is a non-cancerous, triangular-shaped growth that begins on the white surface of the eye (conjunctiva) and spreads onto the cornea. UV sunlight exposure is the primary risk factor for pterygium formation and progression. A pterygium can cause foreign body sensation, irritation, tearing, and redness. These symptoms can be treated by eye drops or ointment prescribed by your doctor at VisionFirst.
However, if a pterygium becomes too large it can cause corneal astigmatism, corneal scarring, and decreased vision. If this occurs, your ophthalmologist will determine whether surgery is needed to remove your pterygium and improve your vision.
Corneal Injury
Chemical Injury
A chemical injury should be treated as a medical emergency that requires immediate attention. Be sure to contact your eye doctor as soon as possible should you sustain a chemical eye injury. There are two types of chemical injury: acid and alkali.
Acid Burns
Acid burns are generally less extensive than alkali burns because acids do not penetrate the eye as deeply.
Common causes of acid burns include:
- Hydrochloric acid found in swimming pools
- Sulfurous acid found in bleach
- Acetic acid found in vinegar
- Hydrofluoric acid found in glass polishing agents
- Alkali Burns
Alkali agents penetrate the eye more deeply and rapidly than acids, resulting in significant ocular damage.
Common causes of alkali burns include:
- Ammonia found in cleaning agents
- Lye found in drain cleaners
- Magnesium hydroxide found in flares and fireworks
- Lyme found in cement and mortar
If you sustain a chemical injury to your eye, it is critical to aggressively irrigate the eye to remove the chemical. If you do not have irrigation fluid available to you, water will work as well. Flush the eye as much as possible and seek immediate medical attention.
Cornea Surgery
The cornea is responsible for refracting light that enters the eye and must be clear for good vision. There are numerous indications for corneal surgery and a variety of different procedures available. If corneal surgery is necessary, our ophthalmologists at VisionFirst will diagnose and guide you through this treatment process.
Cornea Transplant
 Corneal transplantation involves removing the diseased portion of the cornea and replacing it with donor tissue. Both partial and full-thickness corneal procedures are available depending on your condition.
Corneal transplantation involves removing the diseased portion of the cornea and replacing it with donor tissue. Both partial and full-thickness corneal procedures are available depending on your condition.
Penetrating or full-thickness keratoplasty
A full-thickness corneal transplant is commonly referred to as penetrating keratoplasty (PKP). It is performed when the entire cornea is affected by diseases such as a full-thickness corneal scar or advanced keratoconus.
Deep Anterior Lamellar Keratoplasty
Deep Anterior Lamellar Keratoplasty (DALK) replaces the diseased anterior portion or front of the cornea with healthy donor tissue. This procedure is useful in the treatment of keratoconus and corneal scars. Recovery from ALK is often more rapid than full-thickness corneal transplantation.
Descemet’s Stripping and Automated Endothelial Keratoplasty
Endothelial keratoplasty (EK or DSAEK) is used to treat abnormalities involving the posterior or back of the cornea such as Fuchs Dystrophy or bullous keratopathy. Endothelial keratoplasty typically has a more rapid healing time and better visual outcome compared to full-thickness corneal transplantation.
Intacs
Intacs® corneal implants are indicated for the treatment of patients with keratoconus who have experienced a progressive decline in their vision and are no longer able to see well using their glasses or contact lenses. Intacs® are used to reshape or flatten the cornea, with the goal of improving functional vision and delaying the need for corneal transplantation, which is an invasive surgery with prolonged healing time.
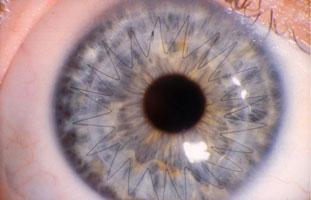
The Procedure
During this in-office procedure, Ophthalmologist will use advanced iFS laser technology to create a pocket or tunnel within the peripheral cornea. Depending on the shape of your cornea, one or two Intacs® will then be inserted into this tunnel, and the procedure is finished. Unlike corneal transplantation, there is no tissue removal and the procedure is reversible.
Intacs® are made of PMMA (polymethylmethacrylate) which is a medical-grade plastic and the same material that has been used for intraocular lens implantation during cataract surgery for more than 40 years. This material has been proven safe and well-tolerated; as a result, it can remain within the cornea permanently.
Recovery
Recovery after Intacs® is fairly rapid, with most patients being able to return to work 1-3 days after the surgery. You will be prescribed topical medications for approximately 2 weeks. Visual recovery is often rapid, but vision can fluctuate for several weeks after surgery as the cornea heals.
If you have keratoconus and are unable to see well using your glasses or contact lens, contact VisionFirst to see if you are a candidate for corneal Intacs®.







