You cannot underestimate the importance of regular eye exams when it comes to caring for your eyes. Many eye diseases such as glaucoma and macular degeneration may not show symptoms early on. A regular eye checkup with VisionFirst Eye Center might prevent these diseases before they become too advanced.
Diabetes
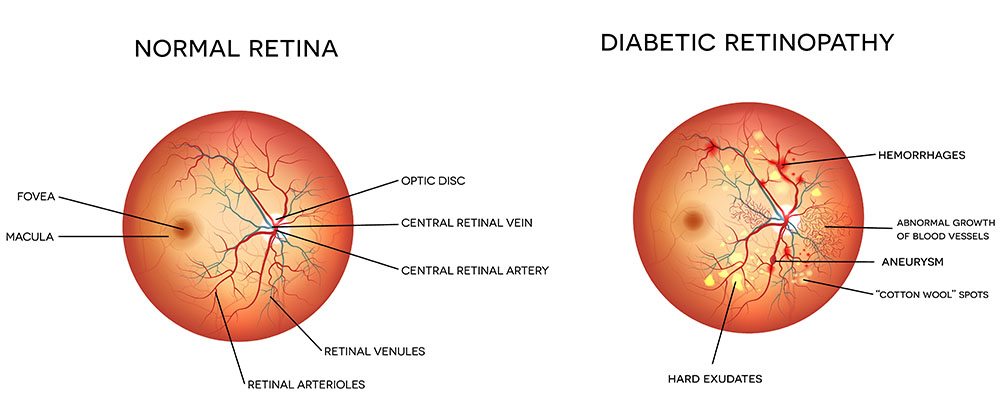
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in American adults. It is caused by changes in the blood vessels of the retina.
In some people with diabetic retinopathy, blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina. The retina is the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision.
If you have diabetic retinopathy, at first you may not notice changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
Testing for Diabetes
Like many other eye diseases, often there are no symptoms in the early stages of the disease, nor is there any pain. Be sure to have a comprehensive dilated eye exam at least once a year.
However, the first symptom you may notice is blurred vision. This may occur when the lens of the eye swells or the macula—the part of the retina that provides sharp central vision—swells from leaking fluid. This condition is called macular edema.
If new blood vessels grow on the surface of the retina, they can bleed into the eye and block vision. At first, you may see a few specks of blood, or spots, “floating” in your vision. If spots occur, see your eye care professional as soon as possible. You may need treatment before more serious bleeding occurs.
Sometimes, without treatment, the spots clear, and you will see better. However, bleeding can reoccur and cause severely blurred vision. You need to be examined by your eye care professional at the first sign of blurred vision before more bleeding occurs.
If left untreated, proliferative retinopathy can cause severe vision loss and even blindness. Also, the earlier you receive treatment, the more likely treatment will be effective.
The test regimen for Diabetes includes:
- Dilated Eye Exam: This test involves putting drops in your eyes to dilate or widen the pupils. This allows your eye doctor to look into your eyes and examine your retina and optic nerve for signs of damage.
- Visual Acuity Test: This is a standard eye test where you look at a chart and measure how well you see at various distances.
- Optical Coherence Tomography: This test is similar to an ultrasound test except that instead of using sound waves to capture images of your tissues, it uses light waves. After your eyes are dilated, you will place your head on a chin rest and hold still while your doctor makes images of your eyes. The light beam does not cause any pain.
Dry Eyes
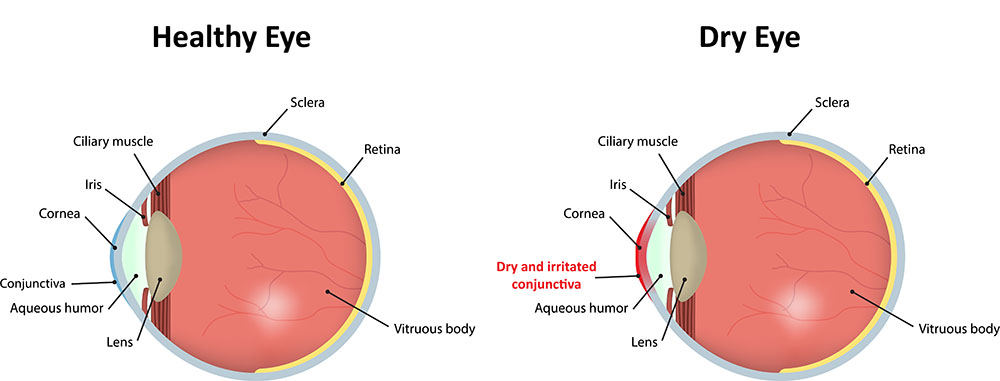
Dry eyes occur when the eye does not produce tears properly, or more commonly when the tears are not of the correct consistency and evaporate too quickly. Inflammation of the surface of the eye may occur along with dry eyes. If left untreated, this condition can lead to pain, ulcers, or scars on the cornea, and some loss of vision. Permanent loss of vision from dry eyes is uncommon.
Dry eye can make it more difficult to perform some activities, such as using a computer or reading. It can decrease tolerance for dry environments or enclosed areas.
Kinds of Dry Eye
Aqueous tear-deficient dry eye is a condition in which the tear glands do not produce enough tears to lubricate the eyes.
Evaporative dry eye may happen when the glands in the eyelids, that make the lipid or oily part of tears, slows evaporation and keeps the tears stable.
Some of the causes of dry eye include:
- Inflammation of the surface of the eye, the lacrimal gland, or the conjunctiva;
- Any disease process that alters the components of the tears; An increase in the surface of the eye, as in thyroid disease when the eye protrudes forward;
- Cosmetic surgery, if the eyelids are opened too widely.
Treatment and Care
Dry eye can be managed as an ongoing condition. The first priority is to determine if a disease is the underlying cause of the dry eye. If so, then the underlying disease needs to be treated.
Cyclosporine, an anti-inflammatory medication, is the only prescription drug available to treat dry eye. It decreases corneal damage, increases tear production and reduces symptoms of dry eye. In some cases of severe dry eye, short term use of corticosteroid eye drops that decrease inflammation is required.
If dry eye results from taking a medication, your doctor may recommend switching to a medication that does not cause the dry eye side effect.
If contact lens wear is the problem, your eye care practitioner may recommend another type of lens or reducing the number of hours you wear your lenses. In the case of severe dry eye, your eye care professional may advise you not to wear contact lenses at all.
Forms of Self Treatment
Use of over-the-counter tears and gels offer temporary relief and provide an important replacement of naturally produced tears. Avoid artificial tears with preservatives if you need to apply them more than four times a day or preparations with chemicals that cause blood vessels to constrict.
Wearing glasses or sunglasses that fit close to the face (wrap-around shades) or that have side shields can help slow tear evaporation from the eye surfaces. Indoors, an air cleaner to filter dust and other particles helps prevent dry eyes. A humidifier also may help by adding moisture to the air.
Avoid dry conditions and allow your eyes to rest when performing activities that require you to use your eyes for long periods of time. Instill lubricating eye drops while performing these tasks.
Glaucoma
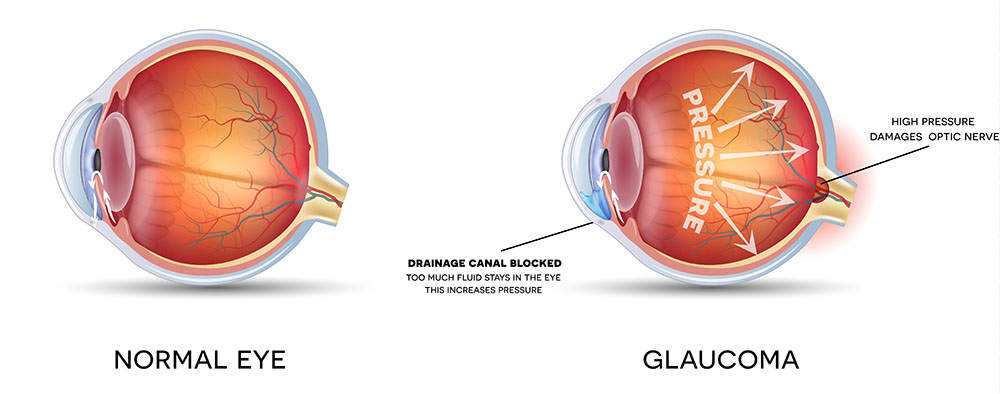
Glaucoma is an eye disease that damages the eye’s optic nerve. That’s the nerve that carries information from the eye to the brain. Left untreated, this disease can lead to vision loss and blindness. Often, you may not know you have glaucoma until it is very advanced. That’s why it is so important to have eye exams on a regular basis.
Glaucoma can sometimes be caused by eye injuries or eye surgery. Even some medications such as corticosteroids can cause glaucoma.
Testing for Glaucoma
There are six tests used to determine if you have glaucoma:
- Dilated Eye Exam: This test involves putting drops in your eyes to dilate or widen the pupils. This allows your eye doctor to look into your eyes and examine your retina and optic nerve for signs of damage.
- Visual Acuity Test: This is a standard eye test where you look at a chart and measure how well you see at various distances.
- Visual Field Test: This test measures the effectiveness of your peripheral vision, or how well you see out of the “corner” of your eye. Often, loss of peripheral vision is one of the first signs of glaucoma.
- Tonometry: Your doctor will measure the pressure inside your eye. High eye pressure may be an indication of glaucoma.
- Pachymetry: Your doctor will apply a numbing drop to your eye then use an ultrasonic wave instrument to measure the thickness of your cornea.
- Optical Coherence Tomography (OCT): This technology scans the nerve layers in the eye, looking for/measuring damage.
Treatment and Care
Most risk factors such as age, race, and family medical history are out of the control of patients. We recommend having a dilated eye exam every 1 to 2 years, especially if you have a family history of glaucoma. There is no restoring vision that is lost to glaucoma so the sooner you treat it the better. Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or it could be a combination of any of these forms of treatment.
Macular Degeneration
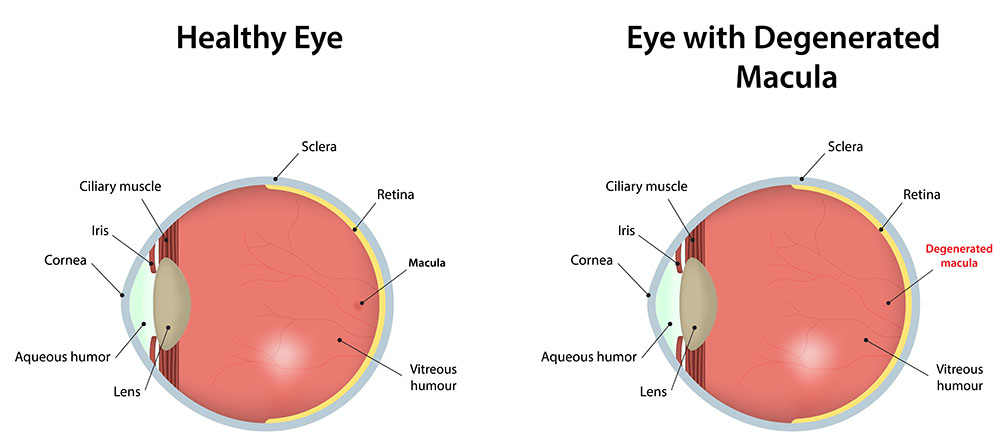
Macular degeneration, also known as age-related macular degeneration or AMD, is a condition where damage has occurred to the macula, a small spot near the center of the retina. The result is a blurry spot in the center of your field of vision. Over time, the blurry spot may grow larger or you may develop blank spots in your vision.
AMD may not necessarily lead to total blindness, but it can affect or limit many activities such as driving, reading, writing, cooking or other types of close work. As you age, the macula can degenerate so that it is less effective in focusing images on your retina.
There are two types of age-related macular degeneration:
- Wet Age-Related Macular Degeneration
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These new blood vessels tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye. Damage to the macula occurs rapidly.
With wet AMD, loss of central vision can occur quickly. Wet AMD is also known as advanced AMD. It does not have stages like dry AMD.
An early symptom of wet AMD is that straight lines appear wavy. If you notice this condition or other changes to your vision, contact your eye care professional at once. You need a comprehensive dilated eye exam.
- Dry Age-Related Macular Degeneration
Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. As dry AMD gets worse, you may see a blurred spot in the center of your vision. Over time, as less of the macula functions, central vision is gradually lost in the affected eye.
The most common symptom of dry AMD is slightly blurred vision. You may have difficulty recognizing faces. You may need more light for reading and other tasks. Dry AMD generally affects both eyes, but vision can be lost in one eye while the other eye seems unaffected.
Testing for Macular Degeneration
- Dilated Eye Exam: This test involves putting drops in your eyes to dilate or widen the pupils. This allows your eye doctor to look into your eyes and examine your retina and optic nerve for signs of damage.
- Visual Acuity Test: This is a standard eye test where you look at a chart and measure how well you see at various distances.
- Amsler Grid: Changes in your vision may cause the lines on this grid to appear wavy or disappear.
- Optical Coherence Tomography: This test is similar to an ultrasound test except that instead of using sound waves to capture images of your tissues, it uses light waves. After your eyes are dilated, you will place your head on a chin rest and hold still while your doctor makes images of your eyes. The light beam does not cause any pain.
Causes
Smoking, race, age, and family history are among the main causes of AMD. The disease is most likely to occur after the age of 60. Having a family history of AMD increases your risk and research has proven that smoking doubles your risk. AMD is also more common among Caucasians.
Treatment and Care
- Dry: Vitamins
- Wet: Injections, Therapy or Laser Surgery
Neurotrophic Keratitis
Neurotrophic keratitis is a disease characterized by decreased corneal sensitivity which can lead to poor corneal healing. It is caused by the loss of sensory function to the ophthalmic portion of the trigeminal nerve, the nerve responsible for sensation and motor functions in the face like blinking and chewing.
This disorder leaves the cornea very susceptible to injury. It also decreases your eye’s natural function of tearing when you blink which can cause severe dry eye syndrome, corneal ulceration, scarring, and vision loss. Herpes zoster, Herpes simplex, and surgery on the trigeminal nerve are the most common etiologies of neurotrophic keratitis.
The ophthalmologists at VisionFirst Eye Center are board-certified and trained in the detection, management, and treatment of corneal diseases including neurotrophic keratitis.







